
Secondary Adrenal Insufficiency

Secondary adrenal insufficiency (SAI) is characterized by a deficiency in the production of adrenocorticotropic hormone (ACTH) by the pituitary gland or CRH by the hypothalamus. The symptoms are the same as for Addison's disease, but in general there is less hypovolemia (Hypovolemia is the state of decreased blood volume, more specifically the volume of blood plasma). The diagnosis is clinical and through laboratory findings, including low plasma concentrations of ACTH and cortisol.
We also have Tertiary IA , but it is still not well
established, with confusion between whether it is a hypothalamus problem
or if it is due to the use of medications (glucocorticoids
and antifungals), being encompassed by most authors in the secondary.
Secondary adrenal insufficiency is the most common type of insufficiency, it can
occurs in:
-
Pan-hypopituitarism
-
Previous chronic hypercortisolism
-
Pituitary tumors
-
Autoimmune lymphocytic hypophysitis
-
Sheehan syndrome
-
Pituitary infiltration or granuloma
-
Isolated congenital ACTH deficiency
The most common cause of secondary adrenal insufficiency is abrupt withdrawal
of exogenous glucocorticoid therapy. During corticosteroid therapy,
of ACTH secretion by pituitary corticotrophs with consequent atrophy
adrenal. Once the supply of exogenous corticosteroids is removed or reduced, the
patient may manifest symptoms of adrenal insufficiency.
Similarly, secondary AI can be seen after treatment of the syndrome
of Cushing.
Symptoms
The signs and symptoms are similar to those of Addison's disease and include:
-
General malaise
-
Asthenia
-
Inappetence
-
Weight loss
-
Gastrointestinal complaints: nausea, vomiting, abdominal pain and diarrhea
-
Hypoglycemia
All signs and symptoms are common in primary, secondary and tertiary failure. However, some symptoms are more suggestive of each of the etiologies, the following stand out in the secondary:
-
Skin pallor in the absence of anemia
-
Secondary hypothyroidism
-
Headache and visual symptoms
-
Diabetes insipidus
A classic difference from Addison's disease and that in secondary adrenal insufficiency we do not have the symptoms of hyperpigmentation and the values are relatively normal for sodium, potassium and urea.
Diagnosis
Laboratory and imaging tests should be performed for diagnosis:
-
Serum cortisol
-
Serum ACTH
-
ACTH stimulus test
-
CNS imaging exams
Confirmatory serum test for secondary adrenal insufficiency.
Patients with confirmed secondary adrenal insufficiency should undergo computed tomography or magnetic resonance imaging of the skull to exclude tumors or atrophy of the pituitary gland.
The CRH test can be used to differentiate between hypothalamic and pituitary causes, but it is rarely used in clinical practice.
Treatment
-
Hydrocortisone or prednisone or prednisolone or dexamethasone
-
Fludrocortisone is not indicated
-
Dose increase during concomitant illness
Glucocorticoid replacement is similar to that described for Addison's disease . Each case varies according to the type and degree of specific hormonal deficiencies.
Most people take the medication three times a day, when they wake up, and then five to six hours a day during the day. The amount and type of medication varies greatly from patient to patient and depends on the type of adrenal insufficiency in which they were diagnosed.
Symptomatic patients should be treated with hydrocortisone or cortisone in the morning and in the afternoon. The goal is to use the lowest possible dose to relieve the patient's symptoms, preventing weight gain and osteoporosis.
During acute febrile illnesses or after trauma, patients receiving corticosteroids for non-endocrine disorders may need supplemental doses to increase their production of endogenous hydrocortisone.
Fludrocortisone is not necessary because intact adrenals produce aldosterone.
In pan-hypophysis, other deficiencies of the pituitary must be treated properly.
Adrenal Crisis / Addisonian Crisis or Acute Adrenocortical Insufficiency
It is the emergency situation of the disease, being potentially fatal.
Without urgent medical treatment, any serious injury or illness can precipitate an adrenal crisis. This can quickly lead to severe hypotension or life-threatening hypovolemic shock.
It may be the first manifestation of adrenal insufficiency or be precipitated by a stressor, such as surgery, infection, trauma, etc.
The crisis occurs mainly in patients exposed to acute stress such as infection, surgery, physical or psychological trauma, salt deprivation, and dehydration due to diarrhea and / or vomiting. In crisis, the carrier feels extremely tired, becomes pale, with fever, low back and abdominal pain, blurred vision, and also has possible fainting, diarrhea, vomiting, tachycardia and / or arrhythmia and dehydration.
Although rare in secondary insufficiency, adrenal crisis can occur. In this case the objective is to reverse the hydro electrolyte imbalance and the deficiency of cortisol.
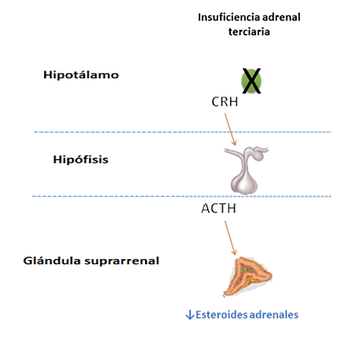
Tertiary Adrenal Insufficiency
We are a family owned and operated business.
Often referred to as secondary, adrenal insufficiency
tertiary care is even rarer than other shortcomings.
It occurs due to deficiency of CRH (hormone releasing
corticotrophin) by the hypothalamus.
The presence of tumors in the hypothalamic-pituitary region or the
its surgical or radiotherapy treatment is an important cause of
IATT due to ACTH deficit, which is usually associated
other pituitary deficiencies.
The hypothalamus is located at the base of the brain, below the thalamus and
above the pituitary gland and is about the size of an almond.
It coordinates most of the endocrine functions, exerting direct action
on the pituitary gland and indirectly on other glands such as adrenals, sexual gonads, thyroid and mammary glands.
It also acts on the regulation of temperature, appetite, thirst, sleep cycle and autonomic nervous system.
Its diagnosis is made by the CRH test, with prolonged and excessive ACTH response, tertiary adrenal insufficiency is confirmed. The test itself may not have useful results due to the large variability in responses related to CRH administration and the cutoff values are not so well defined. Examination such as nuclear magnetic resonance makes it possible to assess the hypothalamus.
We are a family owned and operated business.
The treatment and signs of the disease are the same as for secondary adrenal insufficiency.
